Nearly 50 million Americans suffer from chronic pain—and the search for effective, long-lasting solutions often seems endless. But what if your body could heal from within, making outdated treatments a thing of the past? Stem cell therapy has rapidly emerged as a beacon of hope, offering research-backed breakthroughs for chronic pain sufferers where conventional methods fall short. In this comprehensive guide, we’ll dig into how stem cell therapy is transforming pain management, uncovering everything from clinical evidence and treatment types to patient stories and practical considerations. Let’s explore the new frontier of pain relief.
Stem Cell Therapy: Surprising Impact Backed by Research
- Nearly 50 million Americans live with chronic pain—stem cell therapy offers a new path to relief, far beyond conventional solutions.
Stem cell therapy is reshaping what’s possible in chronic pain relief. More than just another treatment option, this innovative branch of regenerative medicine harnesses the body’s natural repair mechanisms at the cellular level. Recent cell research and clinical trials have demonstrated that stem cell therapy doesn’t just mask symptoms; it can help rebuild damaged tissue, reduce inflammation, and address the root causes of pain. For people suffering from joint injuries, osteoarthritis, or nerve pain, these treatments may offer hope where medications and surgery have stalled.
As new protocols emerge and cell therapies evolve, the conversation is shifting. Patients no longer have to choose between daily medications with side effects and invasive surgeries. Instead, they can look to therapies that stimulate regeneration and healing . Clinical data shows promising results, with many patients experiencing meaningful, long-term relief previously thought impossible. Is this the dawn of a new era in pain management? Research suggests that it very well could be .
How Stem Cell Therapy Addresses Chronic Pain
- Defining stem cell therapy for pain management
At its core, stem cell therapy for chronic pain involves introducing specialized cells into an area of tissue damage or inflammation. Unlike standard pain interventions that aim to play defense—masking symptoms or halting further damage— cell therapy activates your body’s own repair toolkit, enlisting adult stem cells and mesenchymal stem cells to replace, repair, or even regenerate tissue. These cells can develop into various types of tissue, potentially offering relief for complicated musculoskeletal issues and injuries.

- Mechanisms: Stem cell, cell therapy, and regenerative medicine in tissue repair
The mechanisms of action set stem cell therapy apart from other interventions. Upon transplantation, these cells can secrete growth factors, modulate the immune system, and directly participate in tissue reconstruction. For example, mesenchymal stem cells have been shown to reduce inflammation and promote cartilage repair in joint disorders. By intervening at the cellular and molecular level, regenerative medicine offers solutions that could fundamentally change long-term outcomes for chronic pain patients.
- Practical examples of current clinical stem cell treatments
Real-world application ranges from knee osteoarthritis and degenerative disc problems to repairs of rotator cuff and ligament injuries. Many clinics and research centers now integrate stem cell treatments alongside other regenerative procedures like cell transplant and platelet-rich plasma (PRP), offering tailored approaches to complex pain conditions.
What You'll Gain from Understanding Stem Cell Therapy
- A comprehensive overview of stem cell therapy and its capabilities
- An honest look at the types, benefits, and limitations
- Insights into eligibility, process, cost, and long-term expectations
By learning about stem cell therapy for chronic pain, you’ll unlock critical knowledge about the future of pain management. This guide will help you understand the different cell types used in therapy, weigh real benefits against risks, and navigate the complicated landscape of modern cell research . We’ll also address patient eligibility, procedure steps, recovery times, and even costs and insurance factors—equipping you to make informed choices for yourself or your loved ones.
Whether you’re skeptical or optimistic, gaining a clear perspective on the science, evidence, and clinical practice of regenerative medicine will empower you to consider new possibilities for long-term relief. As stem cell therapy continues to mature, being informed is your best first step.
Exploring the Science: What Is Stem Cell Therapy and How Does It Work?
Types of Stem Cells Used in Cell Therapy
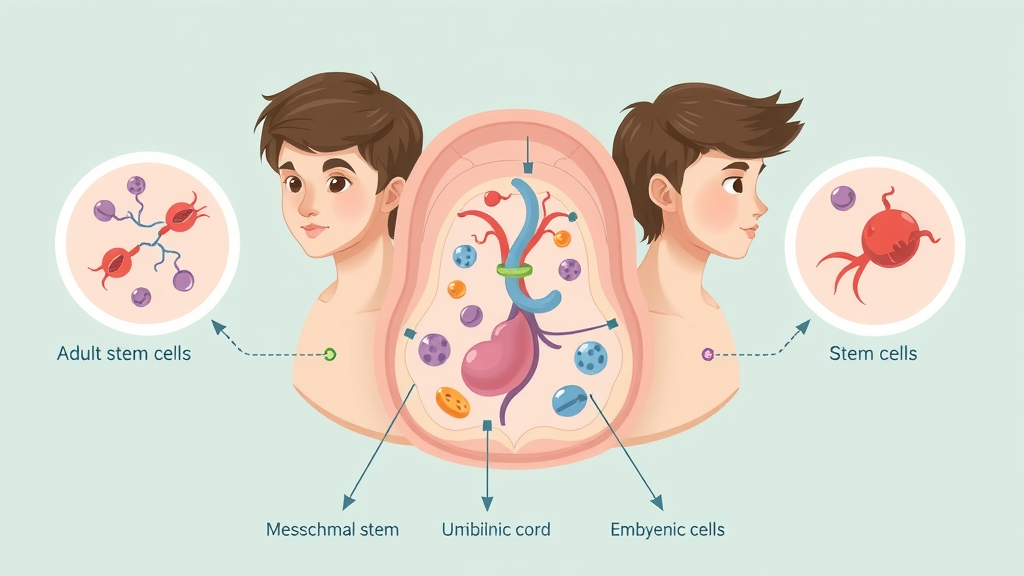
- Adult stem cells, mesenchymal stem cells, umbilical cord, cord blood, embryonic stem cell
Stem cell therapy relies on a range of cell types , each with unique benefits and challenges. Adult stem cells are most commonly sourced from the patient’s own tissues—often from bone marrow or fat. Mesenchymal stem cells are prized for their ability to reduce inflammation and promote tissue repair. Umbilical cord and cord blood provide another rich, ethically neutral source, frequently used in pediatric and research applications. Embryonic stem cells offer the greatest potential for regeneration but are strictly controlled due to ethical considerations.
The use of different stem cells creates flexibility in treatment protocols but also introduces significant variation in efficacy and safety. For chronic pain, adult stem cells and mesenchymal stem cells currently spearhead most clinical applications, thanks to their lower risk of immune rejection and established safety record in cell research and clinical trials .
How Stem Cell Therapies Deliver Regenerative Medicine
- Cell treatment protocols and stem cell research milestones
- Role of bone marrow, stem cell res, and cell transplant
The effectiveness of cell therapy for chronic pain depends on how these cells are sourced, processed, and delivered. Bone marrow-derived stem cell transplants have shown promising results in promoting cartilage repair and reducing pain, particularly in degenerative joint disease. Advances in cell processing and culture ensure that the transplanted cells retain their regenerative potential while minimizing contamination or immune response. Such protocols, underpinned by rigorous stem cell research , are key to optimizing outcomes for chronic pain sufferers.
Recent milestones in cell research include refining delivery techniques (such as direct injection into joints or damaged tissues), enhancing cell viability, and developing personalized cell treatments . Each step moves regenerative medicine closer to mainstream consideration for chronic pain, reducing reliance on invasive surgeries and opioids.
Clinical Evidence: Does Stem Cell Therapy Work?
Results from Clinical Trials and Ongoing Research
- Breakdown of major clinical trial findings
- Latest stem cell research and published results

The question of efficacy is central: Does stem cell therapy actually deliver results for chronic pain? Major clinical trials have shown that, for degenerative joint disease and soft tissue injuries, over 60% of patients report significant improvements after therapy. Clinical studies on knee osteoarthritis, back pain, and neuropathy have produced encouraging results: reduced pain scores, better joint function, and in some cases, avoidance of major surgery.
Peer-reviewed research continually updates the field. Published results highlight both the potential and limitations of stem cell therapy—you’ll find cases of dramatic improvement as well as those where benefits are modest or short-lived. However, the trajectory remains positive, with ongoing trials refining protocols and expanding indications .
"Recent clinical trials show that over 60% of chronic knee pain sufferers experienced significant improvement after stem cell injections."
| Condition | Success Rate (%) | Typical Patient Response |
|---|---|---|
| Knee Osteoarthritis | 60-75 | Pain relief, improved mobility |
| Back Pain/Disc Degeneration | 50-65 | Decreased stiffness, enhanced function |
| Shoulder/Joint Injury | 55-70 | Faster recovery, less inflammation |
| Neuropathy | 45-60 | Reduced tingling, better sensation |
These findings underscore the necessity of personalized treatment plans and further cell research to optimize each application.
Benefits of Stem Cell Therapy for Chronic Pain Management
- Reduction in inflammation, long-term pain relief, tissue regeneration
- Decreased reliance on opioids and invasive surgeries
Clinical trials and case studies consistently report that the top benefits of stem cell therapy for chronic pain include powerful reduction in inflammation, long-term pain relief , and actual tissue regeneration. Compared to steroid injections or pain medications, the regenerative approach seeks to resolve—not just mask—the problem. For patients, this can mean far fewer medications, reduced exposure to the risks of chronic opioid use, and a newfound ability to return to normal activity.
Conditions Best Treated With Stem Cell Treatments
- Knee osteoarthritis, back pain, neuropathy, joint injuries, musculoskeletal conditions
Stem cell treatments are not a one-size-fits-all solution, but clinical data highlight certain chronic pain conditions where results are consistently strong. These include knee osteoarthritis, chronic back pain (especially from disc problems), peripheral neuropathy , and a wide range of musculoskeletal injuries . Even athletes with ligament or tendon injuries are increasingly turning to cell therapies for faster recovery and durability.

Comparing Stem Cell Therapy With Traditional Treatments
| Treatment Type | Approach | Risks/Limitations | Potential for Regeneration |
|---|---|---|---|
| Stem Cell Therapy | Cellular repair & regeneration | Minor procedural risks, cost may be higher | High |
| Physical Therapy | Exercise, manual therapy | Slow progress, may not address severe damage | Low |
| Medications (Painkillers, Steroids) | Symptom relief | Side effects, dependency risk | None |
| Surgery | Structural repair/replacement | Invasive, long recovery, surgical risks | Variable |
While traditional treatments like physical therapy and pain medication offer substantial relief for some individuals, cell therapy stands out for its focus on regeneration and potential for long-term healing . The choice should factor in diagnosis, patient goals, risk tolerance, and careful evaluation of available clinical trial evidence.
Key Cell Types in Modern Cell Therapy
Bone Marrow, Cord Blood, and Umbilical Cord Sources
- Cell transplant types and source matching
- Pros and cons of each stem cell type (adult stem cells, mesenchymal stem cells)
The source of stem cells used in therapy dramatically influences the outcome. Bone marrow–derived stem cells are especially popular due to their established track record and compatibility with adult patients. Cord blood and umbilical cord tissue offer high yields of mesenchymal stem cells ideal for tissue repair and immune modulation, especially in older patients or those with comorbidities.
Choosing the best cell type centers on balancing efficacy, safety, and practical considerations. Pros of bone marrow and adult stem cells include low rejection risk and easy matching for autologous (self) transplant. Mesenchymal stem cells from cord blood have higher regenerative capacities but may have cost or logistical challenges. Every cell transplant protocol requires precise matching and thorough screening to ensure optimal patient outcomes.
Ethical Considerations in Stem Cell Research
- Review of embryonic stem cell and adult stem cell research
- Regulatory landscapes in regenerative medicine

The rapid growth of regenerative med has brought ethical debates to the forefront, especially concerning the use of embryonic stem cells . While adult stem cells and cord blood create fewer ethical dilemmas, embryonic sources are heavily regulated due to moral concerns about embryo use. Regulatory agencies and institutional review boards closely monitor cell research and clinical trials, ensuring that therapies meet ethical and safety standards before public use.
Emerging guidelines in regenerative medicine emphasize patient consent, transparency, and ongoing monitoring for adverse effects. As the field advances, continuous dialogue among ethicists, scientists, and the public shapes how cell therapies will be integrated into standard medical care worldwide.
The Stem Cell Therapy Process: From Consultation to Recovery
- Patient eligibility and screening for stem cell treatments
- Step-by-step breakdown of common stem cell procedures
The path to stem cell treatment begins with detailed screening by a specialist in regenerative medicine. Your eligibility is determined through medical history review, imaging, and sometimes lab work to ensure the best match for therapy and to rule out contraindications.
Once approved, most procedures are performed in an outpatient clinic. After harvesting stem cells (often from bone marrow, fat, or donor cord blood), cells are processed and delivered to the injury site via targeted injection. Patients usually return home the same day, beginning a gradual recovery that may include physical therapy, rest, and return-to-activity guidance from the care team. Most people experience improvements over weeks to months as the **cell treatment** takes effect.
Understanding Risks, Negative Side Effects, and Limitations
- Possible adverse effects: infection, pain, swelling
- Long-term safety evaluations from current clinical trials

Every medical intervention carries some risk, and stem cell therapies are no exception. The most common adverse effects include temporary pain, redness, or swelling at the injection site. Infection risk is relatively low, but it can increase if strict sterility protocols are not followed. Rarely, there may be immune reactions or unintended tissue growth, particularly if cell matching is incomplete.
Most side effects seen in clinical trials are mild and transient. Still, long-term safety data is limited, as stem cell research evolves rapidly. For informed decision-making, it’s crucial that every patient reviews clinical evidence, discusses risks with their provider, and chooses only clinics with rigorous oversight and accreditation in cell therapy .
Success Factors: Navigating Clinical Trials and Treatment Outcomes
- How to interpret clinical trial results in stem cell therapy
- Role of ongoing cell research in improving outcomes
Interpreting clinical trial evidence in cell therapy requires a discerning eye. Not all studies are created equal; look for research that is randomized, controlled, and large enough to reveal real trends. Scrutinize which cell types were used, patient selection criteria, and how outcomes were measured (pain scores, functional testing, imaging results). As the evidence base grows, so does clinician comfort with recommending cell treatments for chronic pain.
The future of stem cell therapy depends on ongoing research. New protocols, better cell processing, and deeper understanding of mechanisms of action all contribute to rising success rates. Patients should be aware that being part of a reputable clinical trial may offer access to next-generation treatments and more comprehensive follow-up.
Cost Analysis and Insurance Considerations for Stem Cell Treatment
| Treatment Area | Average Cost (USD) |
|---|---|
| Knee/Osteoarthritis | $5,000 - $10,000 |
| Back/Spine | $8,000 - $15,000 |
| Shoulder/Joint | $4,500 - $8,000 |
Factors Influencing Price: Procedure, Clinic, and Research Setting
- Insurance, FDA approval, and reimbursement status

The cost of stem cell therapy varies significantly depending on treatment area, clinic reputation, and procedural complexity. While some insurance companies may cover investigational therapy if included in a clinical trial, FDA approval for pain-related stem cell treatment remains limited in the US as of now. Always obtain transparent cost estimates, understand your policy’s boundaries, and weigh potential out-of-pocket costs against expected benefits.
High-quality clinics invest in staff training, advanced facilities, and ongoing research, often justifying higher upfront costs with better oversight and outcomes. If possible, seek referrals or second opinions from board-certified regenerative medicine specialists before committing to a plan.
Expert Insights and Patients’ Real-Life Experiences
"After my stem cell therapy, my knee pain dropped by 80%, and I avoided surgery." — Patient testimonial
- Quotes from orthopedic doctors and regenerative med researchers

Direct patient experiences provide anecdotal confirmation of published results. Many chronic pain sufferers describe measurable decreases in pain, increases in movement, and new hope for full participation in everyday life. Orthopedic specialists and regenerative medicine researchers echo these anecdotes, with experts like Dr. John Michel noting, “Stem cell therapy represents a paradigm shift, transitioning pain management from palliation to true repair.”
All experts emphasize the importance of patient selection and realistic expectations—while most see improvement, a small subset may remain unchanged or only moderately better. Ongoing communication, periodic reassessment, and willingness to integrate other strategies (physical therapy, lifestyle changes) yield the best long-term success.
The Evolution of Stem Cell Research and the Future of Cell Treatments
- Key breakthroughs in stem cell research and regenerative medicine
- Ongoing advancements in cell therapies and treatment indications
Decades of stem cell research have produced remarkable advances, from the first successful bone marrow transplants in hematology to sophisticated mesenchymal stem cell therapies for orthopedics. Continual improvement in cell culture, expansion, and delivery protocols has broadened the scope of treatable conditions and improved outcomes for those battling intractable pain.
The next decade promises further integration of regenerative medicine into mainstream pain care. New frontiers include tissue engineering, gene editing, and hybrid therapies employing both cell treatments and biologic scaffolding. As research continues, patient access is expected to grow, protocols will be refined, and the dream of natural, long-lasting pain relief comes closer to reality.
People Also Ask
What does stem cell therapy do?
Stem cell therapy harnesses unique cells to regenerate tissue and repair damage. It targets the underlying cause of chronic pain, seeking to heal rather than merely mask symptoms.
What are the negative side effects of stem cell therapy?
Potential negative side effects include swelling, redness at the injection site, mild pain, and rarely infection or immune response. Most effects are short-term and manageable.
Does stem cell therapy work for knees?
Clinical evidence and patient outcomes support stem cell therapy as an effective treatment for chronic knee pain, especially for osteoarthritis and cartilage repair.
How long do stem cell injections last?
Relief from stem cell injections can last from six months to several years, depending on the condition treated and the patient’s individual response.
Top FAQs About Stem Cell Therapy for Chronic Pain
-
Who is a candidate for stem cell therapy for pain?
Generally, candidates are adults with chronic pain from joint degeneration, soft tissue injury, or neuropathy who haven’t responded to standard treatments and do not have active cancer or infections. -
Is stem cell therapy FDA approved for chronic pain?
As of now, most stem cell therapies for pain are not FDA-approved outside of clinical trials, but some are allowed or under investigation. Regulatory status may vary with new developments. -
What is the recovery time after a stem cell treatment?
Recovery is usually quick, with most patients returning to non-strenuous activity within a day or two; healing and symptom relief progress over weeks to months. -
How does stem cell therapy compare to PRP (platelet-rich plasma)?
While both aim for regeneration, stem cell therapy introduces new, potent cells for repair, whereas PRP uses concentrated platelets to stimulate healing. The most suitable option depends on the specific condition and severity.
Essential Takeaways for Deciding on Stem Cell Therapy for Chronic Pain
- Stem cell therapy offers clinically-backed, minimally invasive relief for chronic pain
- Outcomes vary, so review clinical trials and consult a regenerative medicine specialist
Ready to Explore Your Options for Natural Pain Relief?
- Reach out to request your complimentary health screening. Call us now at 2816988698
Stem cell therapy is revolutionizing chronic pain management by leveraging the body’s natural healing mechanisms to repair damaged tissues and reduce inflammation. This innovative approach offers a promising alternative to traditional treatments, aiming to address the root causes of pain rather than merely alleviating symptoms.
Key Benefits of Stem Cell Therapy for Chronic Pain:
-
Tissue Regeneration: Stem cells, particularly mesenchymal stem cells (MSCs), have the unique ability to differentiate into various cell types, including bone, cartilage, and muscle. When introduced into damaged areas, they can promote the regeneration of tissues, facilitating healing and restoring function. ( stemcures.com )
-
Inflammation Reduction: Chronic pain is often associated with persistent inflammation. Stem cells possess anti-inflammatory properties that help modulate the immune response, leading to decreased inflammation and, consequently, pain relief. ( orthorepair.com )
-
Minimally Invasive Procedure: Unlike surgical interventions, stem cell therapy is typically administered through injections, making it a less invasive option with reduced risks and shorter recovery times. ( orthorepair.com )
-
Potential for Long-Term Relief: By addressing the underlying causes of pain through tissue repair and immune modulation, stem cell therapy offers the potential for sustained pain relief and improved quality of life. ( medicaltourism.com )
While stem cell therapy presents a promising avenue for chronic pain treatment, it’s essential to consult with healthcare professionals to determine its suitability for individual conditions and to understand the current state of research and regulatory considerations.
 Add Row
Add Row  Add Element
Add Element 



Write A Comment